Iron Deficiency Anaemia (IDA) is the most prevalent nutritional disorder worldwide, affecting approximately 1.92 billion people as of 2021. This condition significantly impacts health, well-being, and economic productivity across both low- and high-income countries.
Understanding Iron Deficiency Anaemia
Iron is essential for producing hemoglobin, a protein in red blood cells that carries oxygen from the lungs to the rest of the body. Iron also supports energy production, DNA synthesis, and the growth and repair of cells. The body regulates iron levels carefully, absorbing a small amount from the diet and recycling most from old red blood cells. A hormone called hepcidin, produced by the liver, helps control this balance by regulating iron absorption and release.
When iron levels drop, the body adapts by reducing hepcidin production, increasing iron absorption from the diet and releasing stored iron. Additionally, low oxygen levels stimulate the kidneys to produce more erythropoietin, prompting the bone marrow to produce more red blood cells.
Acid, particularly gastric acid (hydrochloric acid), plays an important role in iron absorption, complementing the body’s regulatory mechanisms involving hepcidin and erythropoietin. It converts iron to a more soluble form improving its absorption. A reduction in gastric acid secretion, whether due to medical conditions or the use of acid-suppressing medications like proton pump inhibitors, can impair this conversion process, leading to decreased iron absorption and potential iron deficiency anaemia.
Daily iron requirements vary significantly based on age, gender, and physiological state. Adult men typically need 8-10 mg daily, while women of reproductive age require 18 mg due to menstrual blood loss. Pregnant women have the highest needs at 27 mg daily, while children’s requirements range from 7-15 mg depending on their age and growth stage. These increased demands often make it challenging to maintain adequate iron stores through diet alone.
Causes of Iron Deficiency Anaemia
Inadequate Dietary Intake
- Unbalanced diets lacking in iron-rich foods can lead to deficiency.
- Cereal-based diets rich in phytates can inhibit iron absorption.
Blood Loss
- Heavy menstrual bleeding is a common cause in women of reproductive age.
- Gastrointestinal bleeding from conditions like ulcers, gastritis, and cancers can cause chronic blood loss.
- Parasitic infections such as hookworm and schistosomiasis can lead to blood loss, particularly in developing countries.
Impaired Iron Absorption
- Coeliac disease damages the small intestine lining, reducing iron absorption.
- Inflammatory bowel diseases like Crohn’s disease and ulcerative colitis can impair absorption.
- Surgeries such as gastric bypass can also reduce the stomach’s ability to make iron more soluble.
- Proton pump inhibitors (PPIs) are a class of medications used primarily to reduce the production of stomach acid, which can hinder iron absorption.
Increased Iron Requirements
- Pregnancy and breastfeeding increase iron demands to support foetal growth and milk production.
- Children and adolescents may require more iron during growth spurts.
- Endurance athletes may have increased iron needs due to higher red blood cell turnover.
Medication and Lifestyle Factors
- Frequent blood donations can deplete iron stores.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) can cause gastrointestinal bleeding.
- Excessive intake of coffee, tea, dairy or calcium-rich foods can interfere with iron absorption.
Age-Related Factors
- Elderly individuals may experience anemia due to chronic diseases, decreased erythropoietin production, or nutritional deficiencies.
- Chronic conditions such as chronic kidney disease can lead to reduced erythropoietin levels, affecting red blood cell production.
Who’s Most at Risk?
Certain groups are particularly vulnerable to iron deficiency:
Women of reproductive age, largely due to menstrual blood loss and the increased iron demands of pregnancy. As of 2023, about 30.7% of women aged 15–49 worldwide were affected by anaemia.
Young children are another high-risk group. Nearly 40% of children under five had anaemia in 2019. During early childhood, iron is essential for brain development, and a lack of it can lead to lasting cognitive and physical effects.
Teenagers, due to growth spurts.
Athletes, especially endurance runners who lose iron through sweat and minor gastrointestinal bleeding.
People with chronic illnesses that affect nutrient absorption.
Recognising the Symptoms
Symptoms of iron-deficiency anemia can include:
- Fatigue and weakness
- Pale skin
- Shortness of breath
- Dizziness
- Cold hands and feet
- Brittle nails
Some individuals experience unusual cravings for non-food items such as ice, starch, or dirt a condition known as pica. These cravings can serve as important diagnostic clues.
Cognitive symptoms including difficulty concentrating, memory issues, and reduced performance at school or work are often overlooked but can significantly affect quality of life.
Diagnosis of Iron Deficiency Anaemia

According to WHO, anaemia is diagnosed when the concentration of haemoglobin falls below established cut-off values:
- non-pregnant women, 15 years and above - less than 12 g/dl;
- pregnant women - less than 11 g/dl;
- men, 15 years and above - less than 13 g/dl.
Doctors typically start with a complete blood count (CBC), which may reveal small, pale red blood cells (microcytic and hypochromic). Further tests might include:
Serum ferritin (a measure of iron stores). Ferritin is the diagnostic test of choice. Ferritin is also an acute phase protein and is elevated in inflammation, infection, liver disease and malignancy. This can result in misleading elevated ferritin levels in iron deficient patients with coexisting systemic illness. Markers such as C-reactive protein (CRP) may help identify coexisting inflammation. In clinical practice, serum ferritin is a key indicator for diagnosing iron deficiency. For adults, ferritin levels below 30 μg/L are generally indicative of iron deficiency, while in children, levels below 20 μg/L suggest the same. The World Health Organization (WHO) provides more conservative thresholds, defining low ferritin as levels below 15 μg/L for adults and 12 μg/L for children.
Serum iron and transferrin saturation.
Total iron-binding capacity (TIBC).
C-reactive protein (CRP) to assess for inflammation.
Treatment of Iron Deficiency Anaemia
Healthcare providers must investigate underlying causes, which can involve stool testing or endoscopy to detect gastrointestinal bleeding, reviewing menstrual history, or checking for chronic diseases that impair iron absorption or cause ongoing blood loss. Identifying the root cause is key to preventing recurrence. Treatment is with oral or intravenous supplementation.
Definition of Dietary Patterns

Before discussing different types of diets, it is important to highlight that defining dietary patterns such as vegan, lacto-ovo-vegetarian or omnivorous does not in any way determine the quality of the diet. These labels describe what has been excluded from the diet, rather than what is actually included.
As a result, any of these dietary models can be based on refined grains, ultra-processed foods, and low intake of vegetables and fruit, thus ending up being unhealthy and unbalanced.
Unfortunately, most studies do not report the average consumption of each food group within dietary patterns, making it impossible to establish clear correlations.
Iron intake in different dietary patterns
Despite this variability in diet quality, studies have tried to estimate average iron intake across these groups.
Several studies have shown that vegetarians consume an amount of iron equal to or slightly higher than omnivores. A systematic review published in 2021 on the adequacy of vegan diets concluded that several studies found higher iron intake among vegans compared to other diet types. Another notable cross-sectional study involving more than 70,000 participants from the Adventist Health Study-2 found that vegans exceeded recommended iron requirements and had higher iron intake than omnivores.
However, many of these studies did not include biochemical assessments, which prevents evaluating the true prevalence of iron deficiency or iron deficiency anaemia (IDA).
Iron deficiency and IDA: prevalence among omnivores, vegetarians, and vegans
As we mention before, iron deficiency anaemia (IDA) is highly prevalent worldwide, especially among women of reproductive age. For example, in this study involving around 4,000 participants, IDA was found in 6% (using a 12.5 g/dL haemoglobin cutoff), and iron deficiency - in nearly 40% (using a 15 μg/L ferritin cutoff).
As for comparative studies, the most comprehensive to date is a 2017 meta-analysis, which found significantly lower serum ferritin levels in vegetarians (including vegans, lacto-, ovo-, and lacto-ovo-vegetarians) compared to omnivores.
However, this data should be interpreted with caution for several reasons. As we mentioned before, elevated blood ferritin levels often reflect an important marker of inflammation and cellular damage. For this reason, it’s best to check it together with C-reactive protein and other inflammation markers to better understand if low levels are truly due to iron deficiency.
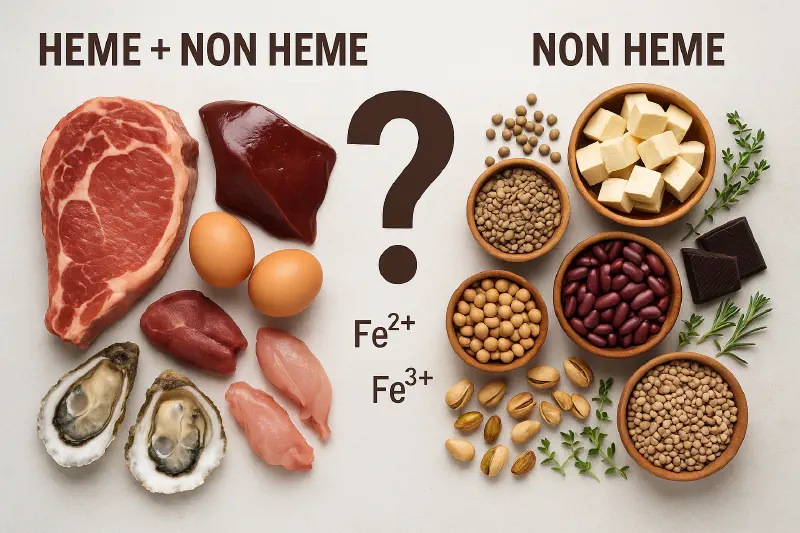
Heme vs. non-heme iron: biochemical differences and average intake across groups
So, what is the main difference between iron from animal foods and plant foods?
The distinction lies in the two forms of iron: heme and non-heme. Animal foods contain both forms in varying proportions, while plant-based foods contain only non-heme iron.
Total heme iron intake in omnivorous diets has been estimated to account for about 5–13% of total iron, with the remainder coming from non-heme sources. Therefore, an adequate intake of non-heme iron is crucial across all dietary patterns.
Heme iron is absorbed more consistently, typically at a rate of 15–35%, whereas non-heme iron absorption varies according to physiological needs and is partially regulated by the body’s iron stores.
A 2013 review found that non-heme iron absorption ranges from 1% to 23%, depending on the individual’s iron status and the presence of absorption enhancers or inhibitors.
Today, it’s well understood that the body can adapt to absorb non-heme iron more efficiently over time. The effects of dietary promoters and inhibitors tend to diminish with prolonged exposure. Individuals with low iron intake can also reduce iron losses to help maintain balance. In one study, total iron absorption increased by nearly 40% after just 10 weeks on a diet with low bioavailability.
This means that people with low iron stores can substantially increase absorption from diets with moderate or high iron bioavailability.
Potential risks of excess heme iron intake
A comprehensive systematic review and meta-analysis of over 400 studies found a strong association between heme iron intake and body iron stores with an increased risk of developing type 2 diabetes mellitus. Notably, none of the studies reported a similar association with total iron intake or iron supplementation.
One proposed mechanism involves the potent oxidative activity of iron. According to this hypothesis, heme iron may promote the formation of highly reactive free radicals, which can damage pancreatic beta cells and impair insulin production and secretion.
Another study, based on Mendelian randomization (a technique using genetic variants to assess cause-effect relationships), showed that a genetic predisposition to higher blood iron levels is associated with an increased risk of type 2 diabetes. Specifically, higher ferritin, serum iron, and transferrin saturation levels were linked to greater risk, whereas markers of low iron status appeared protective.
Factors enhancing or inhibiting non-heme iron absorption
Enhancers of Absorption
Vitamin C (ascorbic acid) enhances non-heme iron absorption by reducing it to a more bioavailable form. Excellent sources include parsley, bell peppers, kiwis, broccoli, cauliflower, lettuce, spinach, citrus fruits, and many other fruits and vegetables, typically abundant in a healthy vegan or vegetarian diet.
Other organic acids, such as citric, malic, and tartaric acids, naturally found in fruits and vegetables, also improve absorption.
Inhibitors of Absorption
Phytates, found in whole grains and legumes, they can bind iron and reduce its absorption. However, because higher phytate intake often coincides with higher iron intake, the negative impact on iron status may be less than expected.
Polyphenols, present in tea, coffee, and wine, can inhibit iron absorption.
Dairy proteins can significantly lower iron bioavailability. Vegetarians who consume large amounts of dairy may thus be at increased risk of iron deficiency.
Calcium: May compete with iron for intestinal absorption. However, studies involving multiple meals suggest that its overall effect is limited.
Preparation techniques
Soaking and sprouting legumes, grains, and seeds can improve iron absorption.
Bread leavening has a similar effect, as do certain fermentation processes, such as those used to make fermented soy products like miso and tempeh.
Dietary sources of iron
To offer a quick comparison, below is a summary of the plant and animal foods richest in iron. It’s evident that many plant foods contain significantly higher amounts of iron than meat.
An often-overlooked source of iron may be culinary herbs, despite the small quantities in which they are typically consumed. For example, two tablespoons of dried thyme provide 12 mg of iron, six times more than 100 grams of beef.
| Food item | Iron (mg per 100g) |
|---|---|
| Dried thyme | 123.6 |
| Dried oregano, dried basil, dried parsley | 41.5–44 |
| Unsweetened cocoa powder | 14.3 |
| Wheat bran | 12.9 |
| Beans, lentils | 8.0–9.0 |
| Pistachios | 7.3 |
| Soybeans, chickpeas, dried peaches, cashews | 6.0–6.9 |
| Muesli, dried apricots, arugula, dark chocolate | 5.0–5.6 |
| Peas, oatmeal, buckwheat | 4.0–4.5 |
| Horse meat | 3.9 |
| Dried plums, durum wheat | 3.6–3.9 |
| Olives, peanuts, dried peaches, millet, soft wheat, hazelnuts, raisins | 3.3–3.5 |
| Cooked lamb | 3.2 |
| Whole wheat flour, almonds, dried figs, spinach | 2.9–3.0 |
| Dates, walnuts, whole wheat bread, corn | 2.4–2.7 |
| Veal | 2.3 |
| Beef, pork, turkey, chicken | 1.6–1.9 |
When choosing dietary sources of iron for everyday meals, it’s important to consider that processed meat has been classified by the IARC (International Agency for Research on Cancer) as a Group 1 carcinogen (known to be carcinogenic to humans), while red meat has been placed in Group 2A (probably carcinogenic).
Moreover, in 2024, a major meta-analysis published in The Lancet explored the link between meat consumption and type 2 diabetes. It examined data from nearly 2 million participants across 20 countries, revealing an increased risk associated with each additional daily portion of both processed and unprocessed red meat, as well as white meat (poultry).
For all these reasons, processed and red meat should be limited in a healthy diet and replaced or complemented with other iron-rich sources.
Conclusion
Iron deficiency anaemia (IDA) is highly prevalent worldwide, especially among women of reproductive age.
The most common causes include malnutrition, low dietary iron intake, heavy menstrual losses, malabsorption, and increased requirements during pregnancy.
In omnivorous diets, heme iron typically accounts for only about 5–13% of total iron intake, with the remaining portion coming from non-heme iron. Therefore, adequate intake of plant-based non-heme iron is essential in all dietary patterns.
Vegans and vegetarians may have lower serum ferritin levels on average. However, this parameter should always be interpreted within the full clinical context. A low-normal ferritin value may reflect low inflammation rather than iron deficiency.
To maintain healthy iron status, vegans and vegetarians should regularly consume iron-rich plant foods.
A well-planned vegetarian or vegan diet should include abundant fruits and vegetables rich in vitamin C and other compounds that enhance iron absorption.
Processed and red meat cannot be considered the primary source of iron in omnivorous diets, as its consumption is associated with increased risks of type 2 diabetes and certain types of cancers. Therefore, it should be limited in a healthy diet.
Individuals with IDA, or those at risk of developing it, should consult their physician and a registered dietitian to determine the underlying cause and develop the most appropriate strategy for prevention or treatment.
Iron supplements should only be used when prescribed by a physician and clinically indicated, based on proper medical assessment.
Discover more: